Apostrophe Treatments
Clindamycin for Acne: Proper Use, Effectiveness, and More
SHARE
Apostrophe Treatments
Clindamycin for Acne: Proper Use, Effectiveness, and More
Medically reviewed by Kristin Hall, FNP
Written by Apostrophe Team
Last updated 4/1/2024
Dealing with acne can be an immensely frustrating experience, especially when your acne is infected and inflamed due to bacteria such as propionibacterium acnes (now called cutibacterium acnes).
Clindamycin is a topical antibiotic that's used to treat many bacterial infections, including the infections that can cause inflamed acne.
It’s fast-acting, easy to use, and effective, making it a good option if you’re prone to pustules, papules, and other inflammatory acne lesions.
Below, we’ve explained what clindamycin is, how it works as an acne treatment, the potential side effects you may experience while using it, and more.
We’ve also listed several other science-backed, proven acne treatments that you may want to consider if you’re prone to acne breakouts.
What is Acne & How Does it Develop?
Before we get into the specifics of clindamycin, it’s important to cover the basics of what acne, or acne vulgaris, actually is, as well as how it can develop on your face and body.
Acne can vary in severity. Comedonal acne lesions, such as whiteheads and blackheads, tend to be small, non-inflamed, and easy to treat.
More severe forms of acne, such as papules, pustules, and nodular or cystic acne lesions, tend to be larger, inflamed, difficult to remove, and painful to the touch.
All acne, whether it’s mild or severe, forms through the same basic process. Over time, sebum -- a type of oil that’s produced by your sebaceous glands -- can build up inside the hair follicles, or pores, in your skin.
When excess sebum mixes with the dead skin cells that build up as part of the skin cell turnover process, it can clog your hair follicles. These clogged follicles turn into acne lesions.
The role of sebum in this process is why acne tends to develop on your face and back -- areas that have lots of oil-producing sebaceous glands.
Enter bacteria. While some acne lesions stay small, others can become large, red, and inflamed as certain bacteria, such as Propionibacterium acnes/P. Acnes (now called c. acnes), multiply inside the clogged hair follicles.
Inflamed, infected acne can range from a few pustules (fluid-filled acne lesions) to large, painful cystic acne lesions.
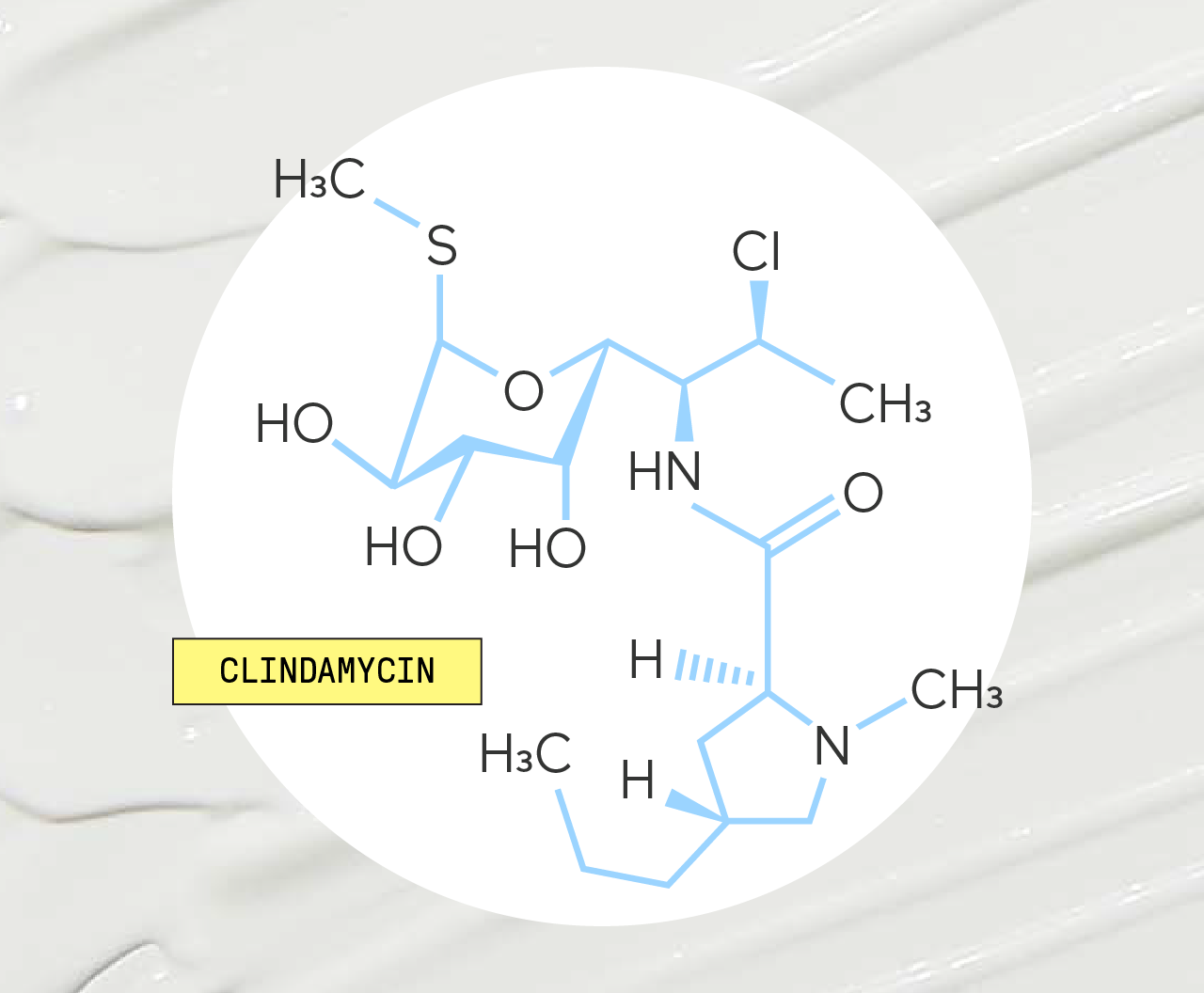
What is Clindamycin?
Clindamycin is a topical antibiotic. It belongs to a class of medications referred to as lincomycin antibiotics and works by preventing acne-causing bacteria from multiplying on your skin.
It also helps to decrease the swelling that often occurs during acne breakouts.
As acne medications go, clindamycin is one of the most direct and effective ways to target and attack the bacteria that make acne such a pain to deal with.
You can find clindamycin in many prescription acne creams and gels. It’s one of several active ingredients in our Customized Acne Cream.
As with many other antibiotics, clindamycin is used to treat a range of bacteria infections. In its oral form, it’s a common treatment for infections of skin, lungs, reproductive system, blood, and internal organs.
How Does Clindamycin Work?
Although bacteria doesn’t cause acne directly, it plays a key role in making acne such a major problem for many people.
Clindamycin helps to reduce the severity of acne by taking certain types of bacteria, such as P. acnes, out of the equation.
As an antibiotic, clindamycin is either bacteriostatic (meaning it stops bacteria from growing) or bactericidal (meaning it kills bacteria directly).
These effects allow clindamycin to stop bacteria from growing inside your pores and causing inflammation.
It’s important to understand that clindamycin doesn’t appear to lower your sebum production or stop dead skin cells from building up on the surface of your skin.
For this reason, it’s not always the best treatment for mild, non-inflamed forms of acne, such as whiteheads or blackheads.
However, if you have inflamed, infected acne, clindamycin is a reliable, effective antibiotic that’s perfect for bringing P. acnes and other types of bacteria under control.
Studies of Clindamycin for Acne
Clindamycin works pretty well, and there are decades of studies showing it. You can start back in the 1980s, where an eight-week study involving more than 300 participants showed that clindamycin reduced acne much, much better than a non-therapeutic placebo.
Like many other acne treatments, clindamycin is often used alongside other medications to treat acne from multiple angles.
Because of this, many studies have looked at clindamycin’s effectiveness as part of a combined acne treatment regimen.
For example, one study published in the Journal of the European Academy of Dermatology and Venereology in 2009 looked at the effects of a two-ingredient acne gel clindamycin and benzoyl peroxide, a popular ingredient in over-the-counter acne products.
The researchers behind this study found that the combination of clindamycin and benzoyl peroxide gel reduced the number of acne lesions and the severity of acne breakouts over 12 weeks.
A different study published in 2015 also found that a combination of clindamycin and benzoyl peroxide produced large improvements in teenagers and young adults with acne, including a significant reduction in the total number of acne lesions.
Finally, a more recent study published in the Journal of Drugs in Dermatology concluded that clindamycin and tretinoin (a topical retinoid that’s often prescribed to manage acne) produced “continuous improvement” in facial acne over the course of 12 weeks of treatment.
In short, several decades of scientific research shows that clindamycin works well, not only on its own, but also when it’s used in combination with other acne medications.
Clindamycin Safety & Side Effects
Topical clindamycin is a safe and effective medication for most people. However, just like other medications, it does have the potential to cause certain side effects.
Most potential side effects of topical clindamycin are mild, but some can be irritating, persistent, and uncomfortable. Common side effects include:
Headache
Dry or peeling skin
Itchy skin
A burning sensation
Newly formed pimples and/or blemishes
If any of these symptoms are severe or persistent, make sure that you contact your healthcare provider.
Although uncommon, clindamycin can cause more serious side effects. You should contact your healthcare provider immediately if you experience watery or bloody stools, diarrhea, or stomach cramps after using clindamycin.
How to Use Clindamycin for Acne
Clindamycin is available as a lotion, gel, foam, or liquid solution. It’s an easy medication to apply to your skin.
If you’re prescribed clindamycin, follow the instructions provided with your medication and apply it to areas of your skin that are affected by acne.
Most forms of clindamycin are intended for use either one or two times per day.
Before applying clindamycin, make sure that your skin is clean. Wash the affected areas of skin with warm water, then gently dry it before applying your medication.
If you normally use other skincare products, make sure to ask your healthcare provider before applying them to skin that’s being treated with clindamycin.
Clindamycin is only safe for use on your skin. Make sure to avoid getting the medication close to or in your eyes, nose, mouth, or areas with broken skin.
If you accidentally apply clindamycin to these areas, make sure to rinse them thoroughly using cool water.
When you aren’t using clindamycin, store it in a secure location away from open flames. Do not smoke while applying clindamycin, as some clindamycin products may be flammable.
If you aren’t sure what to do or have questions about how to use clindamycin, it’s best to talk to your healthcare provider.
Other Medications for Treating Acne
Clindamycin is an effective medication that can reduce inflammation and clear up even the most stubborn acne breakouts. However, it’s far from the only treatment that’s available for acne.
If you have severe or persistent acne breakouts, your healthcare provider may recommend that you use clindamycin with one or several of the following medications:
Benzoyl Peroxide
Benzoyl peroxide is a topical medication for acne. It’s a popular ingredient in acne creams, gels, and lotions sold over the counter.
It works by stopping acne-causing bacteria from growing and, to a lesser extent, by reducing the production of sebum.
Some topical acne products use clindamycin and benzoyl peroxide to target acne from multiple angles at once.
In addition to treating acne more effectively, some research suggests that using these medications together helps to reduce the risk of antibiotic resistance.
Exfoliants
Several exfoliants -- substances that strip away dead skin cells -- are used to treat and manage acne breakouts.
Popular exfoliants include salicylic acid, azelaic acid, glycolic acid, lactic acid and others.
Many of these substances can be found as active ingredients in over-the-counter acne and anti-aging creams.
Tretinoin
Tretinoin is a topical retinoid, a type of medication derived from vitamin A. It works by increasing the speed at which your skin produces new cells and by promoting the peeling of old skin.
Tretinoin is one of the most well-studied acne treatments available. It’s been used for decades, both as an acne medication and as a topical treatment for certain signs of skin aging, including fine lines and wrinkles.
Clindamycin and tretinoin are often used together to treat acne. In one study published in 2011, researchers found that a combination of tretinoin and clindamycin was more effective at getting rid of acne than clindamycin by itself.
Oral Antibiotics
In some cases, your healthcare provider may prescribe oral antibiotics to control and treat your acne.
Several oral antibiotics are used to manage acne, such as doxycycline, minocycline, amoxicillin, erythromycin, and trimethoprim.
These medications are generally used for moderate or severe acne that doesn’t clear up with topical treatments.
Isotretinoin
Isotretinoin is an oral retinoid. It’s a powerful medication that’s often prescribed to treat severe, stubborn acne that doesn’t improve with other medications.
In a 2009 study, topical clindamycin and isotretinoin proved effective as a combined treatment for moderate acne.
Your healthcare provider may recommend using these medications together if you have nodular acne, cystic acne or other severe acne that doesn’t seem to respond to other treatments.
Lifestyle Changes & Habits
Although lifestyle changes and good skin care habits aren’t a medication per se, they can make a big difference to the appearance of your skin and the severity of your acne.
In addition to using medication, your healthcare provider may suggest lifestyle changes, dietary approaches or simple skincare habits that you can use to reduce your risk of developing acne breakouts.
It’s important to follow your healthcare provider’s instructions and implement every approach to treat acne, whether it’s the use of medication, lifestyle changes or both.
The Bottom Line on Clindamycin and Acne
As a topical antibiotic, clindamycin is a valuable acne-fighting tool that’s particularly effective for treating and preventing infected, inflammatory acne breakouts.
If you have moderate to severe acne, your healthcare provider may suggest using clindamycin either on its own or in combination with other medications to manage your breakouts and clear your skin.
If you’re prescribed clindamycin or a combination medication that contains clindamycin, make sure to use it exactly as instructed.
Over time, you may start to notice fewer pimples, less severe acne breakouts and clearer skin, even in areas that used to be prone to acne.
If you’d like to use clindamycin or similar medication to improve your skin, you can view our full range of skin care products online.
Get your own Apostrophe Customized Acne Cream, which could contain clindamycin based on what your provider thinks is the best fit for your skin.
You can learn more about the best ways to control acne breakouts and maintain clearer skin in our guide to prescription acne medication.
14 Sources
Acne. (n.d.). Retrieved from https://www.americanskin.org/resource/acne.php
Clindamycin Topical. (2016, October 15). Retrieved from https://medlineplus.gov/druginfo/meds/a609005.html
Clindamycin. (2018, May 15). Retrieved from https://medlineplus.gov/druginfo/meds/a682399.html
Murphy, P.B., Bistas, K.G. & Le, J.K. (2020, June 28). Clindamycin. StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK519574/
Becker, L.E., et al. (1981, August). Topical clindamycin therapy for acne vulgaris. A cooperative clinical study. Archives of Dermatology. 117 (8), 482-5. Retrieved from https://pubmed.ncbi.nlm.nih.gov/6455095/
Ko, H.-C., et al. (2009, March). Prospective, open-label, comparative study of clindamycin 1%/benzoyl peroxide 5% gel with adapalene 0.1% gel in Asian acne patients: efficacy and tolerability. The Journal of the European Academy of Dermatology and Venereology. 23 (3), 245-50. Retrieved from https://pubmed.ncbi.nlm.nih.gov/19438817/
Kaur, J., Sehgal, V.K., Gupta, A.K. & Singh, S.P. (2015, May-August). A comparative study to evaluate the efficacy and safety of combination topical preparations in acne vulgaris. International Journal of Applied & Basic Medical Research. 5 (2), 106–110. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4456883/
Solna, M.A., et al. (2019, April). Observational Study of Clindamycin Phosphate and Tretinoin Gel for the Treatment of Acne. Journal of Drugs in Dermatology. 18 (4), 328. Retrieved from https://jddonline.com/articles/dermatology/S1545961619P0328X
Matin, T. & Goodman, M.B. (2020, November 24). Benzoyl Peroxide. StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK537220/
Leyden, J. & Levy, S. (2001, February). The development of antibiotic resistance in Propionibacterium acnes. Cutis. 67 (2 Suppl), 21-4. Retrieved from https://pubmed.ncbi.nlm.nih.gov/11236211/
Tretinoin Topical. (2019, March 15). Retrieved from https://medlineplus.gov/druginfo/meds/a682437.html
Schmidt, N. & Gans, E.H. (2011, June). Clindamycin 1.2% Tretinoin 0.025% Gel versus Clindamycin Gel Treatment in Acne Patients. The Journal of Clinical and Aesthetic Dermatology. 4 (6), 31–40. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3140902/
Sutaria, A.H., Masood, S. & Schlesinger, J. (2020, August 8). Acne Vulgaris. StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK459173/
Sardana, K., Garg, V.K., Sehgal, V.N., Mahajan, S. & Bhushan, P. (2009, May). Efficacy of fixed low-dose isotretinoin (20 mg, alternate days) with topical clindamycin gel in moderately severe acne vulgaris. Journal of the European Academy of Dermatology and Venereology. 23 (5), 556-60. Retrieved from https://pubmed.ncbi.nlm.nih.gov/19143903/
Shop this post

Clindamycin
Like what you just read? Sign up for our email list to get the scoop on skincare science delivered straight to your inbox.

Education
What is milia?
What is milia? Today, we’re jumping into one type of bump that you may have heard about most commonly in infants — milia.
Read More
Education
Best moisturizer for acne-prone skin
If you have combination acne-prone skin, figuring out which moisturizer is best for your skin might be tough. In this guide, we break down the best moisturizer for combination, acne-prone skin.
Read More
Education
How to build a face care routine
As you get into skincare, it might seem overwhelming, especially trying to figure out the order you're supposed to apply products in. Below, we detail how to build a face care routine for your skin!
Read More

